[Updated January 10, 2019]
If eyes are the windows to the soul, then the ears are its curtains: Whether they are minimalist Roman shades or fringed swags that would make Scarlett O’Hara blush, a dog’s ears frame her face and set off her expression. In other words, while they have a utilitarian function (and an important one at that) they have a cosmetic one, too. So imagine my dismay when I noticed that my handsome old Rhodesian Ridgeback, Blitz – he of the two gorgeously symmetrical triangles held crisply and smartly against his graying face – had what appeared to be a frankfurter growing on the edge of his right ear.
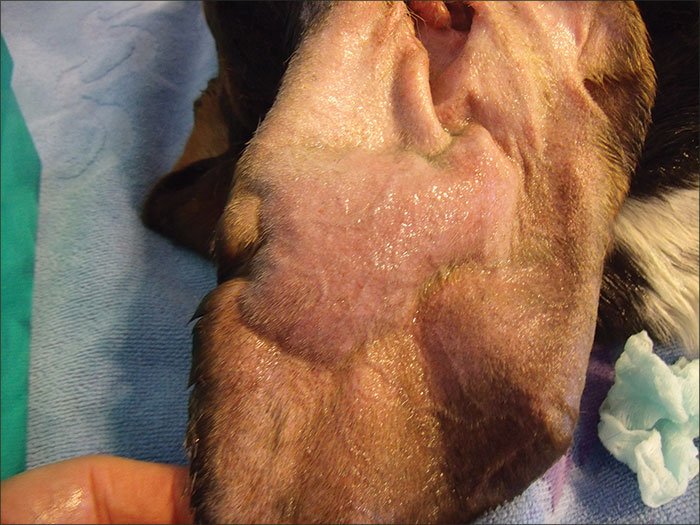
The purplish, sausage-like lump turned out to be an aural hematoma. An accumulation of blood in the ear flap resulting from a broken blood vessel, hematomas are common in drop-eared breeds like mine, though they occur in dogs of all ear types. They are believed to be caused by trauma to the relatively thin tissue of the ear flap, or pinna, often as a result of head-shaking.
The good news about hematomas is that, if left untreated, they are eventually reabsorbed. They will not burst – even though by all appearance they look ready to pop – and the dog is left no worse for wear, except for having to endure the discomfort of a large blood blister weighing down her ear. (There is a great diversity of opinion about just how painful ear hematomas are for dogs, and the only ones who know for sure aren’t talking.)
The bad news is that allowing nature to take its course can have aesthetic implications: As the blood-filled ear flap heals and contracts, scar tissue often develops, causing thickening and wrinkling that make it often noticeably different from its non-clotted counterpart. It’s sort of the doggie version of “cauliflower ear” in boxers (the pugilists, not the canines), whose battered outer ears can become swollen and misshapen, resembling the texture of the vegetable that lent its name to the condition.
In Blitz’s case, I took him to a veterinarian whose expertise in traditional Chinese medicine I greatly admire. But acupuncture and herbs were not options in this case. “Chinese medicine is good for a lot of things,” the vet said with a smile. “But not everything.” His preferred treatment for aural hematomas was to insert a small drain into the ear, which we did. Blitz’s hematoma eventually resolved, and his ear was slightly smaller and a little thicker than it had been before. Not an ideal outcome, but not a terrible one, either.

That seems to be the general theme when it comes to aural hematomas: There are many different methods for treating them, and none is perfect. The overriding challenge is that the hematoma separates the skin from the ear cartilage – sort of like a calzone, to use another food comparison. The inability to get those layers to reattach is what causes the ear to shrivel and become misshapen.
Below are some methods for treating hematomas. Some are mainstays that most veterinarians will recognize; others are relatively new approaches that try to maximize the effort to get the skin and cartilage to start talking to each other again, and one has been used as far back as the time of the Pharaohs – on humans, at least. Remember, though, that taking action is a choice, not a necessity: If you’re okay with that frankfurter shriveling up into a cauliflower, then you can do nothing. Your dog probably couldn’t care less.
Early Intervention
For those who like to incorporate alterative modalities into their dog’s health care, holistic medicine offers maddeningly few options for quickly clearing up hematomas to avoid scarring. Shawn Messonnier, DVM, of Paws & Claws Animal Hospital in Plano, Texas, says he has had “pretty good success” using the homeopathic remedies hypernicum and arnica on smaller hematomas – those that take up one-fourth or less of the ear. “Very often those remedies will help resolve hematomas when they are really small,” he says. But as time progresses, and the hematoma begins to clot and harden, homeopathy can be less effective.
Because eosinophils (a type of white blood cell), and mast cell infiltrations have been found in hematomas, some experts speculate that the blood blister may be a component of an allergic reaction. Veterinarians who use only conventional medicine sometimes prescribe steroids such as prednisone to reduce inflammation, though a 2011 review of treatments for aural hematomas in dogs for the Evidence-Based Veterinary Medical Association found the effectiveness of steroids in resolving hematomas and preventing their recurrence to be inconclusive. Some practitioners use cold-laser treatments to help shrink the hematoma and destroy inflammatory cells.

Ways to Treat a Dog’s Ear Hematoma
Dr. Leni Kaplan, a faculty member in the Community Practice Service of Cornell University College of Veterinary Medicine in Ithaca, New York, says if she does decide to treat a hematoma, she will insert a small sterile tube to help the ear drain. (Some vets use a specific draining tube called a cannula; Dr. Kaplan prefers a bovine teat cannula, used to treat mastitis in cows, or just sterile IV tubing sewn inside the ear.)
More important than the kind of drain used is the follow-up care that the dog receives. “The main thing is that the owners have to gently massage the ear” to keep the hematoma draining, Dr. Kaplan explains. “If the owner the doesn’t do any home care, it’s a bloody mess.”
The purpose of a drain or cannula is to keep fluid moving out of the hematoma so that it reduces in size, but a downside is that this method doesn’t do much to compress the skin and cartilage together.
A new surgical approach by Rachel Seibert, DVM, and Karen M. Tobias, DVM, DACVS, at the University of Tennessee, takes the idea of having an active drain a step further by creating negative pressure to constantly suck out liquid even as it brings the separated layers together. With their technique, a large needle is inserted into the hematoma to empty it, then a vacutainer (a sterile tube that creates a vacuum so blood can be drawn out easily) is attached to the ear using a butterfly catheter.
“We started using this technique because it is less invasive than surgery, does not require general anesthesia, and has a similar success rate to surgery without the risks,” Dr. Seibert explains. “The reason this technique works is that it is successful at maintaining contact between the skin and cartilage with constant negative suction.”
Dr. Seibert says the success rate with the negative-pressure drain is similar to treatment with drainage followed by steroid injections, with a recurrence rate of 22 percent. “The pinna is typically minimally distorted or wrinkled using this technique,” she says, “and most cases should resolve within seven to 10 days.”
Though the technique is fairly straightforward, challenges include successfully bandaging the whole affair so that it stays on but doesn’t restrict the dog’s breathing; and making sure the owner replaces the tube at regular intervals, because once it fills to a certain point, suction is impaired.
Surgical Removal of Ear Hematomas
In the quest to get the skin and cartilage of the ear to reattach, many (if not most) veterinarians opt for surgery. The drawback to any kind of surgery is that the dog must undergo anesthesia, and post-operative recovery is relatively more painful.
The procedure involves opening the hematoma surgically with an incision on the inner flap of the ear running in a wavy line; the incision drains the hematoma. Then the incision is stitched up, and more stitches are used in what looks just like a “quilting” technique, with knots on both sides of the ear flap, preventing any part of the ear flap from puffing up with fluid again. Many small stitches are used so there are no large unstitched areas where the blood can accumulate again. (Some vets actually stitch shirt buttons to both sides of the ear to exert more and wider pressure on the flap, literally pressing it together!)
Tina Wolfe, DVM, of Poland Veterinary Centre in Poland, Ohio, prefers the incisional method for a hematoma that is chronic – when it has become firm as a result of clotting and is beginning to be reabsorbed.
“The incisional technique allows for a more complete evacuation of the hematoma once a significant clot has formed, which can help decrease the rate of recurrence,” she explains, noting that the sutures help to promote scar tissue and decrease the space for an additional hematoma to form.
For acute hematomas, where a significant clot hasn’t yet developed, Dr. Wolfe opts for a different surgical technique. With a small skin-biopsy punch – which is traditionally used to extract small circles of tissue to be sent to a laboratory for analysis – she makes a series of small staggered holes along the hematoma on the inner surface of the ear flap. After the hematoma has drained, she places a single stitch through each of the small hole punches, tacking the exposed cartilage to the skin without closing the hole.
Newly formed acute hematomas “are more soft and fluid in nature and will drain readily though the biopsy sites, which allows for continued drainage of the hematoma,” she explains. “The punch-biopsy method also tends to have a high success rate, is quickly and easily performed, and has a good cosmetic result.”
As with the quilting technique, no bandages are necessary, though an Elizabethan collar or other protective device is recommended to make sure the dog does not scratch or shake the ear.
“I prefer either of these techniques to drainage alone or cannulas due to higher rates of success and cosmetic outcomes,” Dr. Wolfe concludes. “Both the incisional and punch-biopsy methods have a lower rate of recurrence than cannulas and needle drainage because the sutures help to promote scar tissue and decrease the space for an additional hematoma to form.”
In a paper published in July, Drs. András Gyorffry and Attila Szijártó of Semmelweis University in Budapest, Hungary, outlined still another operative technique for aural hematomas. With this approach, the hematoma is opened with an incision on the inner flap of the ear running perpendicular to the ear tip. Absorbable sutures that run parallel to the wound are then placed inside the ear tissue, binding together the cartilage and subcutaneous tissue, but not penetrating the skin. After all the stitching is done, the two edges of the incision do not meet, but rather are left a millimeter or two apart, permitting fluid to continue to drain as the ear heals from the inside out.
In a retrospective study of 23 dogs with aural hematomas that were treated with this technique between 2006 and 2012, the authors reported that all but two – or more than 90 percent – healed without any deformity to the ear, and none required additional surgery or had a recurrence. The two cases of misshapen ears were due to a bacterial infection in one and misaligned stitches that permitted wrinkling in the other.
“The new method offers a minor risk of postoperative complications while accomplishing high healing rates,” the authors concluded in their paper.
Leeches for Ear Hematomas
We’ve saved the best – or at least, the most unconventional – for last. In a word: leeches.
These slithery, blood-sucking worms have been used for centuries, dating back to ancient Egypt. Even today in human medicine, leeches are used to drain pooled blood after a digit has been surgically reattached, to treat varicose veins and blocked arteries, and to lessen pain from osteoarthritis. And in dogs, they are most commonly used to treat ear hematomas.
Shelley R. Epstein, VMD, CVH, of Wilmington Animal Hospital in Delaware, has blogged about her experience with leech therapy, formally called hirudotherapy. “No anesthesia is needed; the leeches inject a numbing chemical into the site,” she writes. “It may take a month for the hematoma to fully heal, but the ear is usually normal in appearance afterward.”
According to Biopharm in Hendy, South Wales (“suppliers of leeches since 1812”), ear hematomas in dogs usually call for two to three leeches, and the sooner they are applied, the better. “Leeches can still be used on hematomas that are slightly older and firmer, but in these cases two leech treatments may be required in order to best decongest the blood,” the company explains on its web site. After the leeches are removed, the wound can continue to bleed steadily for as many as 10 hours – ideal in the case of hematomas, where active drainage is needed.
Biopharm describes leeches as “perfectly designed” sucking machines. Leeches have three sets of jaws containing approximately 100 teeth each, and leave a bite mark that resembles the Mercedes-Benz emblem. Along with the natural anesthetic that helps dull the pain of their initial chomp, leeches release several compounds when feeding, including hirudin, an anti-coagulant that maintains blood flow during feeding; and calin, which inhibits clotting for a period afterward. Biopharm acknowledges that as with any treatment, there is a risk of allergic reaction or infection, but notes that it is rare.
In the United States, medicinally farmed leeches are considered a “medical device” by the Food and Drug Administration (FDA), and their use is regulated by federal law. “Vets have ordered from us,” a terse-sounding spokesperson from Leeches U.S.A. in Westbury, New York, told us; she did not know for what purpose the leeches had been ordered.
Leeches are used for only one treatment, and most meet their demise thereafter. In Dr. Epstein’s practice, they are “retired, and kept in a bowl to swim around.”
The Bottom Line
In the end, it can seem there are as many ways to treat hematomas as there are dogs who develop them. And, depending on whom you talk to, the end results can vary dramatically.
Even though surgery is said to be the best method to avoid scarring and malformation, “I’ve see the ones that have gone to surgery and half of those are as scarred down as those that haven’t,” Dr. Kaplan observes. “And I’ve seen ones where the owners did nothing and their ears look great.”
Still, there are a few constants when it comes to caring for a dog with a hematoma:
If you opt for veterinary intervention, seek it out sooner rather than later, before the hematoma hardens and becomes more difficult to treat.
After the insertion of a device or procedure to drain the hematoma, be meticulous about after care, following your vet’s instructions to keep the hematoma draining and stop fluid build-up.
Avoiding further concussion to the ear is vitally important if it is to stabilize and heal. As annoying or awkward as it is, be sure your dog wears some type of Elizabethan collar to deter scratching and minimize the effects of shaking.
Treat the underlying cause of the head-shaking that produced the hematoma. Otherwise, you are only addressing the symptom and not the cause.
If Blitz were around today, and I had another shot at treating his hematoma, I’d likely pursue some of the newer treatments outlined in this article. Heck, I might even give leeches a try. I’d like nothing better than to find an approach that actually works for this infuriating ear condition – and to keep that head “drapery” as handsome as ever.
Don’t Shake Your Head!
Though the cause of hematomas hasn’t been definitely identified, most veterinarians point to head shaking as the likely culprit. Vigorous or repeated head-shaking can cause a blood vessel in the ear flap to burst and cause acute swelling – but we’ve also seen dogs whose own ID tags have injured their ear flaps during head shaking, initiating the hematoma spiral. So, to keep hematomas from recurring – and to avert their formation in the first place – it’s important to get to the root cause of head shaking and resolve it.
Ear infections are a prime cause of head shaking, and can be persistent and difficult to treat. But once the infection has been brought under control, your work is not done: You need to find out of the source of the imbalance that produced the infection to begin with. Pay attention to whether there has been a change in the dog’s food, supplements, or probiotics; I noticed that even changing my dogs’ diet from raw to home-cooked resulted in an uptick in occasional ear infections.
Another, less obvious cause of head shaking – and the likely cause in Blitz’s case – is a lack of household humidity. Especially in wintertime, household air tends to dry out, and with it the dogs’ skin. An increase in dander makes them itchier, which in turn makes them shake more.
Running a humidifier, boiling a kettle of water, or simply leaving a bowl of the wet stuff out atop a radiator and regularly refilling it can restore much-needed moisture to the household – and stop Fido from flapping.






I quit this article once i reached the suggestion that traditional chinese medicine can work.
For an animal lover to support such a barbaric and inhumane industry is nonsensical.
Too bad Carl, the article is very informative. The author presents the discussion in a very well rounded manner. The treatments are described much more and thoroughly than most articles I have read, some 1000 articles. I am a researcher and medical device provider for a non-surgical treatment for aural hematoma, the Auralsplint. The one common among the articles is the lack of a treatment to heal all the problems associated with surgery. The hematoma in itself is bad, but surgery is invasive and outright gruesome. I realize the DVM’s are trained to perform surgical remedies, and get paid to do so. To agree with you, this surgery is barbaric. This is precisely why I invented the Auralsplint, patented it in 2006, and now offer it as a medical device to the industry, and to the animal owners at large. It is a must to provide to the public an alternative, especially one that works to solve the problems spoken of here. I hope you fully read the article after reading this response, and find I am correct and you are correct, and the author is correct in her attempt to inform the public.
The published “Auralsplint – Descriptive Report” is linked to Auralsplint.org on the Veterinary Portal page. 5-year study ending in 2017.
strangely i have had a sub chorionic hematoma- one that surrounds the uterus when pregnant! it was over 14 cm large and could have been very serious for the baby life. i did go to my acupuncturist and she worked on my blood disorder and blood flow. in 2.5 weeks my ultra sound showed the hematoma went from 14cm to 3cm. i wasn’t doing anything else except taking calcium and magnesium.
even though I’m a human, i believed it was almost solely from opening up the blood flow in my body. i also think this comment from carl may have more biased around it then it being an actual fact that chinese medicine is barbaric. I’ve never heard of such a thing.
You should have read the 2nd sentence where the Chinese vet says “Chinese medicine and herbs were good for some things but not everything… not for dog hematomas” !!!!!
The Chinese medicine is Younan Baiyou. It was recommended by my dogs oncologist for stopping a bleeding tumor. I believe it is saving his life
Very wide used be vets.
Ya I quit going to college as soon as I read about having to read about stuff.
Proper relief for draining the hematoma is a hypodermic needle aspiration. The hematoma will refill due to the broken blood vessels are still broken. Instead of continued aspirations, you should use an auralsplint to secure the ear flap while healing occurs. Details at Auralsplint.org or Facebook at Auralsplint.
Is there any Homeopathic remedies to treat such ailments.Can you suggest some of the names.
Try HAMPL
We experienced this with our then 9-year-old Ridgeback. We had always been careful to avoid ear-scratching, head-shaking, etc… knowing full well hematomas were a thing with our breed. My husband was a wrestler throughout his life, and had lots of experience with understanding ear hematomas, cauliflower ear, etc… we just could not find a vet who would listen. The first one didn’t even examine our dog, just started lecturing us about ear infections -which our dog had never had, in his whole life. He wasn’t interested in helping the situation, only in making money treating invented underlying causes. Our dog never scratched and rarely shook his head. He woke up that morning with the hematoma after going to bed just fine the night before. He yelped when getting out of his crate, and that’s how we discovered the trauma. We had been playing Frisbee, as we often did, and he bounced around, shaking the disc, also usual. I initially thought that was the cause, but after our dog later died, I have to wonder if he had one of two underlying genetic disorders, or if the loads of pain medications he was on for his ear after a different vet opted to do the “quilting” procedure and drains was the culprit. He was 6 weeks short of his 10th birthday when he passed.
We avoided the surgery as long as we could, but after a couple of months, with no change, he was scheduled to undergo removal of a mole on his eyelid that had begun to interfere with his vision and eye health, so the vet went ahead while he was under and did the ear, too. I had, until then, been using arnica, researching many alternative medicines and options, and doing my best. Poor guy was definitely in pain no matter what, and being the one who had to keep maintaining the drain and opening up the wound to allow it to continue to flow instead of filling back up… it was not easy on either one of us. If I had it to do all over again, I would have just left it alone. Maybe he would have lived a little longer.
Finding a vet who is willing to listen to the humans, consider all options, etc… is not an easy thing. We were new in town, besides, and had no idea what vet to choose, after moving away from a decades-long relationship with our former vet clinic.
I always appreciate Denise Flaim’s articles and expertise! I have followed her writing for many years! I would love to read more about correlations re: Ridgebacks, hematomas, and the relationship to possible genetic blood disorders.
Hi Jennifer
I just noticed my almost 10 year old Pitt bull terrier’s white ear as I was bathing her with a hematoma. She has had 2 others on her other ear (the blue one) which was relieved with surgery and a cannula. Did great !!!! But now at her age I don’t want surgery if possible. She suffers with skin allergies put since Apoquel she’s been doing well. She is cared for and watched 24/7 sound would have noticed if she were scratching. Anyway I’m mortified !!!! It’s 1:40 AM and I don’t know which way to go. As with ur pup I couldn’t bear losing her under anesthesia at her age. Any suggestions PLEASE. BTW I’m not concerned about how her ear looks after the fact…fixing the problem in her best interest is my main concern. Thanks to all and any comments.
If you have been aspirating by hypodermic needle to keep the bubble deflated, then you may be a candidate for the Auralsplint.
how do o use a needle to drain hematoma in my elderly lab had surgery years ago expensive using zymax in ear for mites and warm cloth on his ear thinking about giving arnica
try a mixture of : cod liver oil , honey , essential oil of Arnica , and turmeric powder . It reduced a large hematoma on my dogs ear by 30-40 percent in less than a week .
Hi! This sounds so promising, and I’d love to try it on my dog. This might be a dumb question, but did you have your dog ingest this mixture or did you topically apply it to the ear? Thanks in advance!
I’m wondering the very same thing!!! Did you figure it out?
Thanks Eric! But please tell us the proportions & how to use the mixture. I just paid a mint to have the hematoma surgically corrected, but I can feel the hard places in my dog’s ear forming. And she’s shaking her head probably because that ear itches. I didn’t want to get the surgery, but I also didn’t want her ear to heal with a lump in it. Your natural treatment is more in line with my ideas on how to treat her & can only help even if she is post-op now. Thanks again!
I just discovered a hematoma on my 13+ year old dog’s ear. I really don’t think this is something to present to a Vet, especially involving a surgical procedure. He shows no pain from the area. He does not shake or scratch his head any more than he has ever done. If I had to guess, I believe he may have received it from laying on the wood floors for hours on end. His ears are not the same. One ear is upright (German Shepard) and the other droops (Rottweiler). Too much info, I know. I really just would like verification on leaving a 13+ year old dog ear untreated.
My dogs was there for a week and the day before I was about to take him to his appointment at the vet it ruptured so I wouldn’t say it’s not possible!
Honestly, surgery should be discussed and researched before use. Vet clinics are not in the business of medical dressings and will promote surgery because it generates the most revenue. However, aural hematoma in dog is curable without surgery, with a holistic medical device and dressing called the Auralsplint. Auralsplint Inc. PBC provides this Class 1 medical treatment custom kits to those in need and can be delivered in 1-2 days USA. In short, the auralsplint provides pressure against he broken b blood vessels and holds the tissue in close proximity while healing occurs naturally. Simple and effective and available to you at Auralsplint.org.
The bottom line is taking good care of your dog’s and cat’s ears with treatment of any ear infection or disease reduces head shaking which is what causes ear (aural) hematomas to begin with. Determining which treatment to use depends on the severity of the hematoma. Infection can cause the problem to become worse, causing the tissue to die, leaving the owner the only option then of frequenting a veterinary professional. So, whether you tend to it yourself or go to a veterinarian, making sure the process stays clean and as bacteria free as possible benefits you and your dog or cat.
My dog got an ear hematoma last week, playing with another dog. Rushed her to ER vet. They tried to drain it but it was too painful, so they put her on Prednisone 10mg for 7 days and then a tapering dose for the next 7 days. Well, it’s no longer painful but it’s still there. We are in the second week now, tapering the Prednisone. I cannot stand the side effects at 10mg. The tapering dose is half of that. Trying like heck to get in to see a holistic vet but no one has any openings for a month. It’s really frustrating. Never heard of this problem until a week ago
what were the side effects? my dog has one likely from shaking her head from allergies. the vet gave her ear drops and prednisone but not quite as long as u. she seems so tired and her belly is rumbling. i’ve read about using traumeel cream on them but i havent tried it.